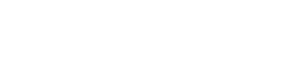
In a world where technological and scientific advances continue to redefine what is possible in public health, the resurgence of malaria in Africa is a glaring and avoidable crisis. Since 2020 the global burden of malaria has continued to rise. The number of cases reached 263 million in 2023 (rising by 11 million from 2022), with the largest increases concentrated in Africa (accounting for 89.7% of the global rise).1 These figures underscore the urgent need for intensified malaria control efforts, particularly in regions affected by conflict, vulnerable to climate change, and where health systems are under strain. After decades of progress, this disease is making a dangerous comeback—fuelled by drug resistance, climate change, weakened health systems, and dwindling global financial commitment. If we fail to act collectively now, we risk reversing hard won gains and jeopardising the health and future of millions of people across the continent.
In 2023 malaria killed nearly 600 000 people in Africa—95% of global deaths from this preventable and treatable disease
In 2023 malaria killed nearly 600 000 people in Africa—95% of global deaths from this preventable and treatable disease.1 The continent also recorded 246 million cases, and between 2022 and 2023, several countries experienced surges in cases, highlighting both the scale and geographic spread of the challenge. Ethiopia, for example, reported an estimated 4.5 million additional cases.1 But what alarms us most is not just the scale of the disease—it is that malaria is spreading into previously non-endemic regions or countries that had a low disease burden. As of June 2025 several southern African countries are experiencing a sharp rise in malaria cases and deaths compared with the same period in 2024.2 Zimbabwe has reported 111 998 cases and 310 deaths, a dramatic increase from 29 031 cases and 49 deaths the previous year.2 In Botswana, cases surged from 218 to 2223, with 11 deaths reported—up from none in 2024.2 These trends highlight the urgent need for cross-border coordination, enhanced surveillance, and targeted vector control to prevent further escalation. The threat is evolving. Our response must evolve with it.
One of the most worrying developments is the emergence of partial resistance to artemisinin based combination therapies (ACTs)—our first line of defence against malaria. Studies in Ethiopia, Rwanda, Tanzania, and Uganda confirm rising resistance.3 This threat could erode decades of medical progress and lead to higher mortality unless it is quickly contained through improved genomic surveillance, evidence based drug policies, and strict treatment adherence.2
Malaria resurgence is also being amplified by climate related changes and the aftermath of the covid-19 pandemic, which disrupted routine health services and diverted resources
Malaria resurgence is also being amplified by climate related changes and the aftermath of the covid-19 pandemic, which disrupted routine health services and diverted resources.4 Insecticide treated nets, indoor spraying, and seasonal chemoprevention efforts have stalled or regressed in several regions.5 Funding gaps have widened. And although we now have two approved malaria vaccines—RTS,S/AS01 and R21/Matrix-M—countries in southern Africa that are currently reporting outbreaks have yet to introduce them.6
This must change. At Africa CDC, we are calling for a continent-wide response that is anchored in five key priorities. Firstly, we need to revitalise genomic surveillance and research. We must strengthen local research institutions so that African scientists are empowered to lead context specific innovations, from vector control strategies to drug resistance monitoring. Understanding the patterns of drug resistance and parasite mutations is crucial. By scaling up pathogen genomics initiatives—particularly through regional genomics sequencing hubs—we can enable real time tracking of malaria transmission patterns, mutations, and emerging threats. Data alone, however, are not enough. They must be integrated into decision making processes through strong health governance, cross-sector collaboration, and evidence informed policy frameworks.
At Africa CDC, we are calling for a continent-wide response that is anchored in five key priorities
Secondly, disease surveillance and reporting need to be strengthened. Timely detection and responses are hindered by several persistent challenges. These include limited diagnostic capacity at the community level, under-reporting because of weak health information systems, and inconsistent data quality across regions. Insecurity and geographic inaccessibility in conflict affected or remote areas further disrupt case detection and follow-up. In addition, the flow of data between public, private, and informal health sectors is fragmented, often resulting in incomplete surveillance coverage.
These challenges are compounded by shortages of trained personnel and limited integration of real time data into decision making processes. Africa must digitise and modernise how we detect and respond to outbreaks by using platforms like DHIS2 and enhanced Integrated Disease Surveillance and Response—starting with primary healthcare centres that are accessible to the community.
Thirdly, malaria vaccines should be rolled out equitably. No child should die of malaria when effective vaccines exist. We call on our partners and governments to accelerate the introduction and uptake of malaria vaccines, particularly in high risk and underserved regions. Public health efforts also need to reinforce proved prevention tools such as vector control measures, including indoor spraying, insecticide treated nets, and community engagement.
Africa’s malaria response must be led and owned by Africans
Finally, Africa’s malaria response must be led and owned by Africans. Sustainable financing is crucial to realising this goal, and we urge countries to meet the Abuja declaration’s target to allocate 15% of national budgets to health.7 Implementing innovative domestic financing mechanisms, such as solidarity levies and excise taxes (taxes on airline tickets, imports, alcohol, tobacco, and mobile services) would help to meet this goal. Where donor funding supports malaria control and prevention, it should be aligned with national malaria priorities to ensure programmes are sustainable and effective.
Eliminating malaria by 2030 is not a distant dream. It is a realistic and attainable goal—but only if we act decisively. Malaria is a measure of the global community’s commitment to equity, innovation, and solidarity. As we face new biological and environmental threats, eliminating malaria will prove that we can overcome even our most entrenched public health challenges—together. Africa has shown resilience and determination in the fight against HIV, Ebola, and covid-19. With the right investment, collaboration, and leadership, we will do the same with malaria.
*Jean Kaseya, Director General, and Nebiyu Dereje, Head of the Division of Knowledge Management and Policy Translation and Editor-in-Chief, are affiliated with the Africa Centres for Disease Control and Prevention and the Journal of Public Health in Africa, respectively.
References
- World Health Organization. World malaria report 2024. www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2024.
- Africa CDC. Malaria surge in Southern Africa. 23 Jul 2025. https://africacdc.org/news-item/malaria-surge-in-southern-africa
- Rosenthal PJ,
- Asua V,
- Bailey JA,
- et al
- The emergence of artemisinin partial resistance in Africa: how do we respond?Lancet Infect Dis2024;24:e591-600. doi:10.1016/S1473-3099(24)00141-5 pmid:38552654CrossRefPubMedGoogle Scholar
- Kaseya J,
- Dereje N,
- Tajudeen R,
- Ngongo AN,
- Ndembi N,
- Fallah MP
- . Climate change and malaria, dengue and cholera outbreaks in Africa: a call for concerted actions. BMJ Glob Health2024;9:e015370. doi:10.1136/bmjgh-2024-015370 pmid:38453519FREE Full TextGoogle Scholar
- Namuganga JF,
- Epstein A,
- Nankabirwa JI,
- et al
- . The impact of stopping and starting indoor residual spraying on malaria burden in Uganda. Nat Commun2021;12:2635. doi:10.1038/s41467-021-22896-5 pmid:33976132CrossRefPubMedGoogle Scholar
- ↵World Health Organization. WHO recommends R21/Matrix-M vaccine for malaria prevention in updated advice on immunization. 2 Oct 2023. www.who.int/news/item/02-10-2023-who-recommends-r21-matrix-m-vaccine-for-malaria-prevention-in-updated-advice-on-immunization
- ↵African Union. Abuja declaration on HIV and AIDS, tuberculosis and other related infectious diseases. 2001. https://africanlii.org/akn/aa-au/statement/declaration/2001/hiv-aids-tuberculosis/eng@2001-04-27